Anthem Blue Cross Provider Appeal Form
Anthem Blue Cross Provider Appeal Form - When the provider disagrees with an anthem blue cross billing determination. If yes, designation of representation (dor) form must be signed by the patient and submitted with this request if not already submitted. If anthem blue cross and blue shield healthcare solutions has rendered an adverse determination for either an administrative or medical. Use the provider dispute resolution request form: Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient. Use this form only to request an appeal for medical necessity for which you have received an initial denial letter from utilization management. If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. A payment appeal is defined as a request from a health care provider to change a decision made by anthem blue cross and blue shield healthcare.
Use this form only to request an appeal for medical necessity for which you have received an initial denial letter from utilization management. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient. When the provider disagrees with an anthem blue cross billing determination. If yes, designation of representation (dor) form must be signed by the patient and submitted with this request if not already submitted. Use the provider dispute resolution request form: If anthem blue cross and blue shield healthcare solutions has rendered an adverse determination for either an administrative or medical. A payment appeal is defined as a request from a health care provider to change a decision made by anthem blue cross and blue shield healthcare. If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals.
If anthem blue cross and blue shield healthcare solutions has rendered an adverse determination for either an administrative or medical. If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. Use this form only to request an appeal for medical necessity for which you have received an initial denial letter from utilization management. If yes, designation of representation (dor) form must be signed by the patient and submitted with this request if not already submitted. Use the provider dispute resolution request form: When the provider disagrees with an anthem blue cross billing determination. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient. A payment appeal is defined as a request from a health care provider to change a decision made by anthem blue cross and blue shield healthcare.
Anthem Blue Cross Provider Manual 2024 Pdf Free Sibyl Kristien
When the provider disagrees with an anthem blue cross billing determination. If anthem blue cross and blue shield healthcare solutions has rendered an adverse determination for either an administrative or medical. If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. A payment appeal is.
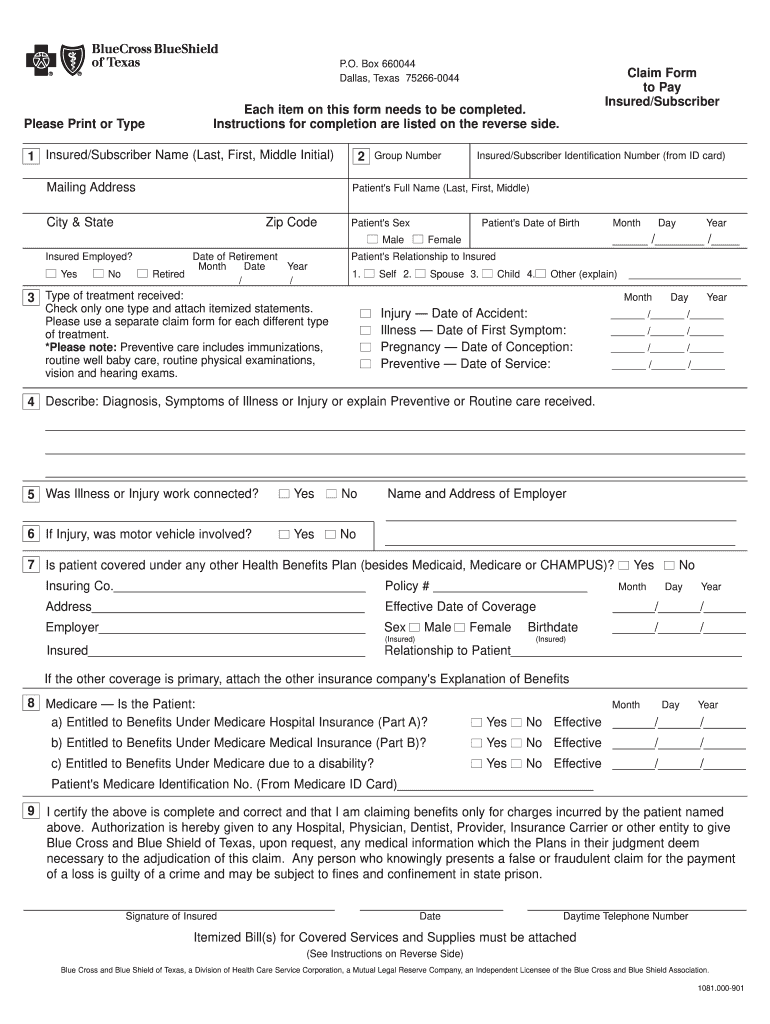
Blue Cross Blue Shield Claim Edit & Share airSlate SignNow
Use this form only to request an appeal for medical necessity for which you have received an initial denial letter from utilization management. If anthem blue cross and blue shield healthcare solutions has rendered an adverse determination for either an administrative or medical. Use the provider dispute resolution request form: If a provider does not agree with the outcome of.
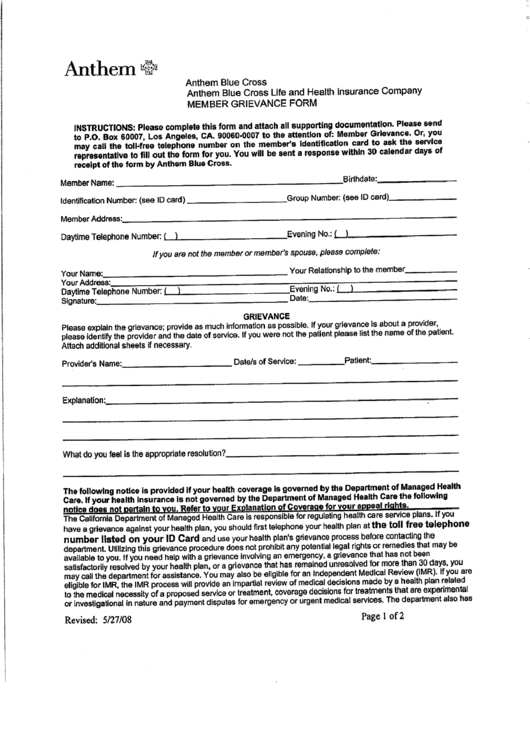
Anthem Blue Cross Member Grievance Form printable pdf download
Use the provider dispute resolution request form: If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. When the provider disagrees with an anthem blue cross billing determination. If yes, designation of representation (dor) form must be signed by the patient and submitted with this.
Anthem provider appeal form pdf Fill out & sign online DocHub
If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient. Use the provider dispute resolution request form: If yes, designation of representation (dor).
Anthem Blue Cross Member Services Provider Medicaid BCBS www
When the provider disagrees with an anthem blue cross billing determination. Use the provider dispute resolution request form: If yes, designation of representation (dor) form must be signed by the patient and submitted with this request if not already submitted. Use this form only to request an appeal for medical necessity for which you have received an initial denial letter.
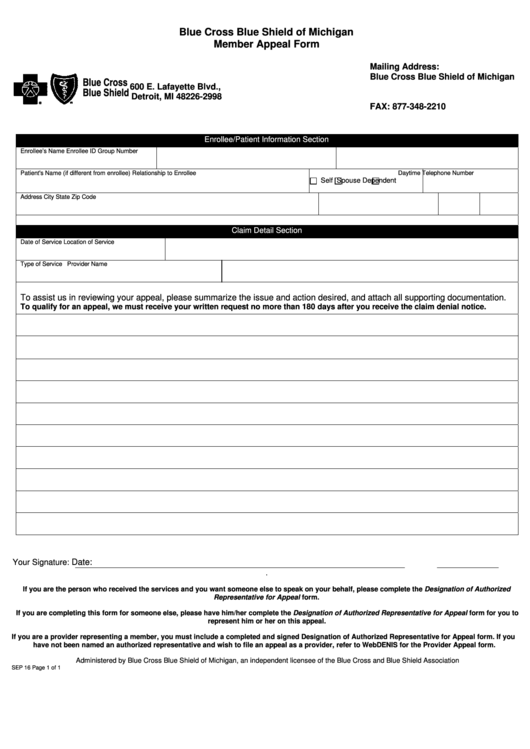
Fillable Blue Cross Blue Shield Of Michigan Member Appeal Form
A payment appeal is defined as a request from a health care provider to change a decision made by anthem blue cross and blue shield healthcare. If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. When the provider disagrees with an anthem blue cross.
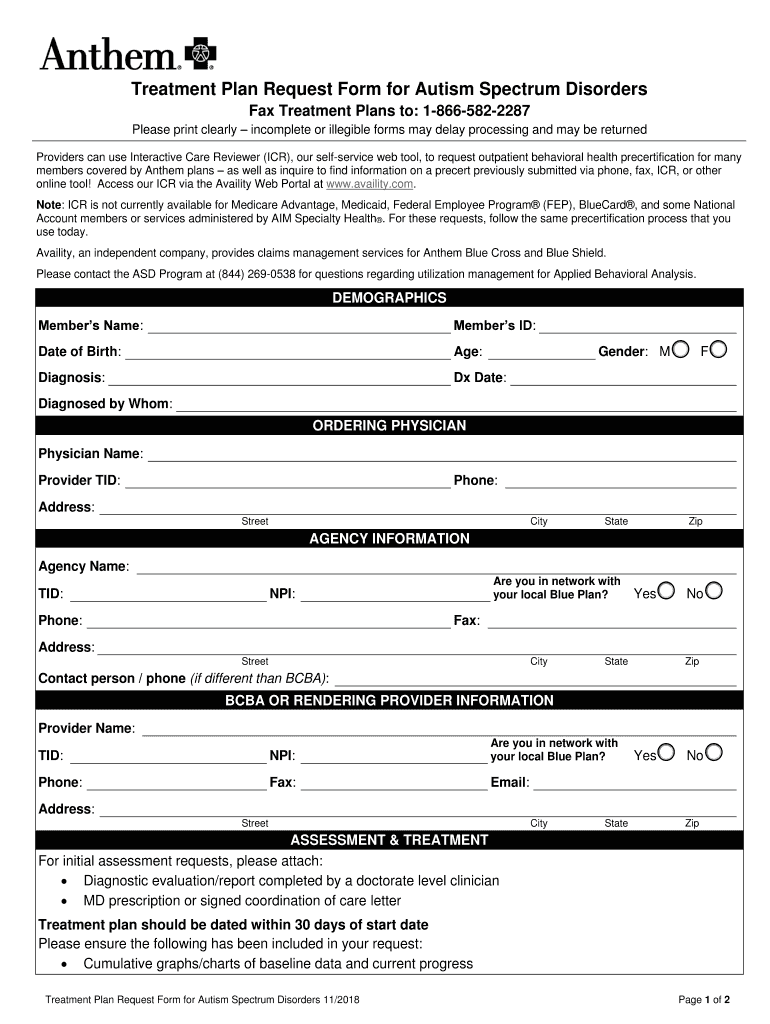
Anthem Treatment Plan Request Form for Autism Spectrum Disorders
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient. Use the provider dispute resolution request form: If yes, designation of representation (dor) form must be signed by the patient and submitted with this request if not already submitted. Use this form only to request an appeal for.
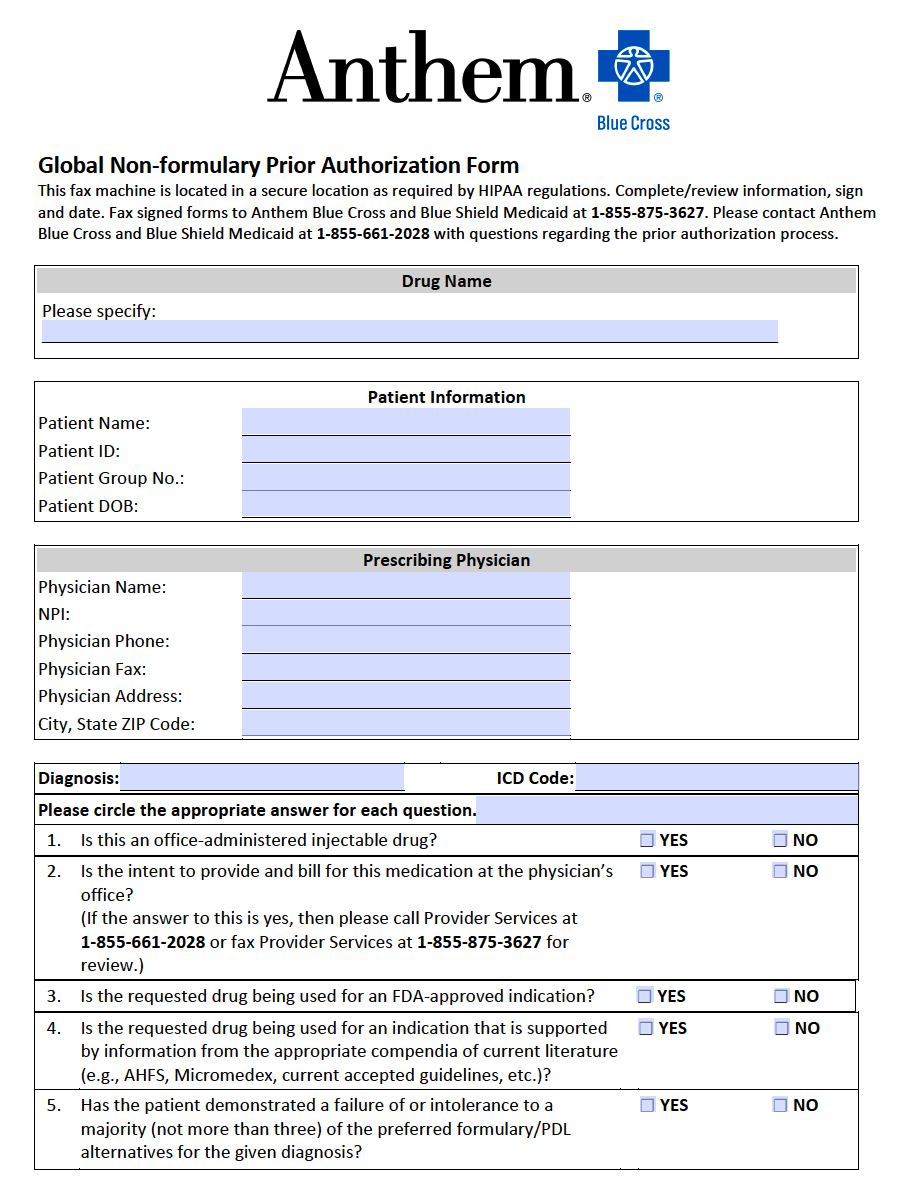
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. When the provider disagrees with an anthem blue cross billing determination. Use the provider dispute resolution request form: If yes, designation of representation (dor) form must be signed by the patient and submitted with this.
Anthem Blue Cross Provider Manual 2024 Pdf Free Sibyl Kristien
A payment appeal is defined as a request from a health care provider to change a decision made by anthem blue cross and blue shield healthcare. If yes, designation of representation (dor) form must be signed by the patient and submitted with this request if not already submitted. When the provider disagrees with an anthem blue cross billing determination. Use.
Anthem Blue Cross California Grievance Form Blue Cross Blue Shield
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient. A payment appeal is defined as a request from a health care provider to change a decision made by anthem blue cross and blue shield healthcare. Use this form only to request an appeal for medical necessity for.
A Payment Appeal Is Defined As A Request From A Health Care Provider To Change A Decision Made By Anthem Blue Cross And Blue Shield Healthcare.
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient. If anthem blue cross and blue shield healthcare solutions has rendered an adverse determination for either an administrative or medical. When the provider disagrees with an anthem blue cross billing determination. Use the provider dispute resolution request form:
If Yes, Designation Of Representation (Dor) Form Must Be Signed By The Patient And Submitted With This Request If Not Already Submitted.
If a provider does not agree with the outcome of a claim determination, the provider may appeal the decision by using the claim payment appeals. Use this form only to request an appeal for medical necessity for which you have received an initial denial letter from utilization management.