Meridian Of Illinois Prior Authorization Form
Meridian Of Illinois Prior Authorization Form - Use this form to ask us to make a coverage determination and/or prior authorization. Determine if a pa is needed with the meridian prior auth check tool. Prior authorization form standard/urgent requests: Use the tool below to see if prior authorization (pa) is needed. How to request a prior authorization. Each link will open a new window. Submit pas electronically through the. If an authorization is required, submit a request using the secure provider. You do not need a paper. Once you have completed and signed this form,.
Each link will open a new window. Once you have completed and signed this form,. You do not need a paper. Use this form to ask us to make a coverage determination and/or prior authorization. You must include the most recent relative laboratory results to ensure a complete pa. Use the tool below to see if prior authorization (pa) is needed. Determine if a pa is needed with the meridian prior auth check tool. If an authorization is required, submit a request using the secure provider. How to request a prior authorization. Prior authorizations cannot be completed over the phone.
How to request a prior authorization. Each link will open a new window. Use the tool below to see if prior authorization (pa) is needed. Determine if a pa is needed with the meridian prior auth check tool. You do not need a paper. If an authorization is required, submit a request using the secure provider. Some covered services or medications may need approval from meridian, and this is called a prior authorization (pa). Prior authorizations cannot be completed over the phone. Prior authorization form standard/urgent requests: You must include the most recent relative laboratory results to ensure a complete pa.
Meridian Health Plan Illinois Prior Authorization Form
You must include the most recent relative laboratory results to ensure a complete pa. Use the tool below to see if prior authorization (pa) is needed. Once you have completed and signed this form,. Use this form to ask us to make a coverage determination and/or prior authorization. Each link will open a new window.
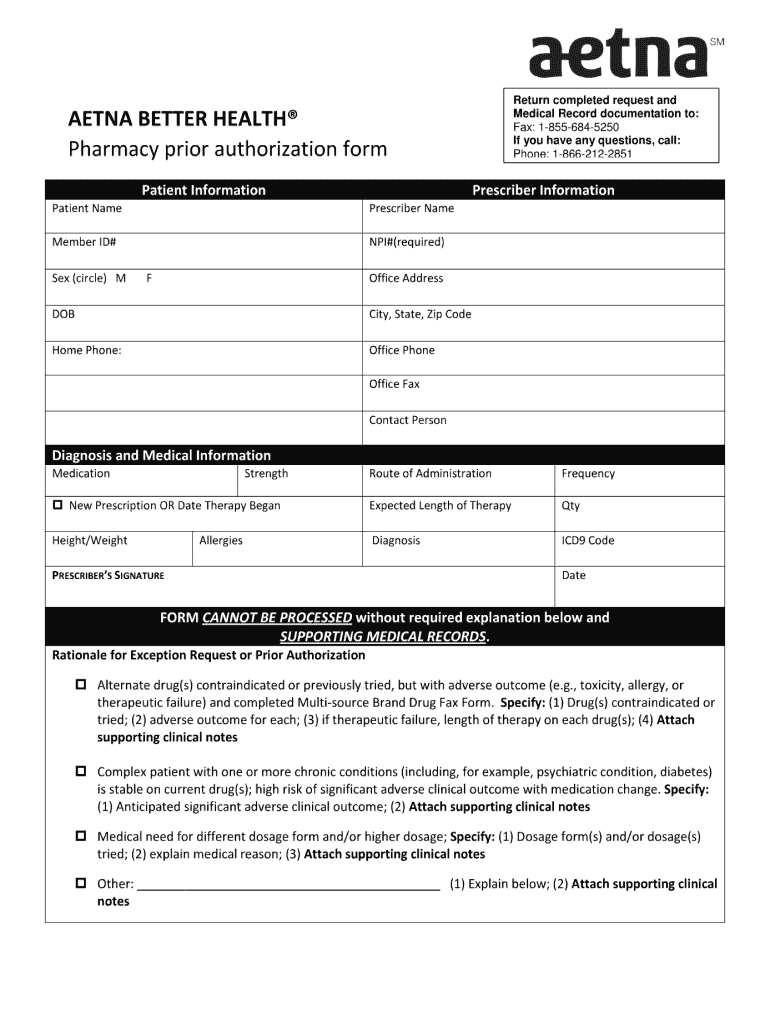
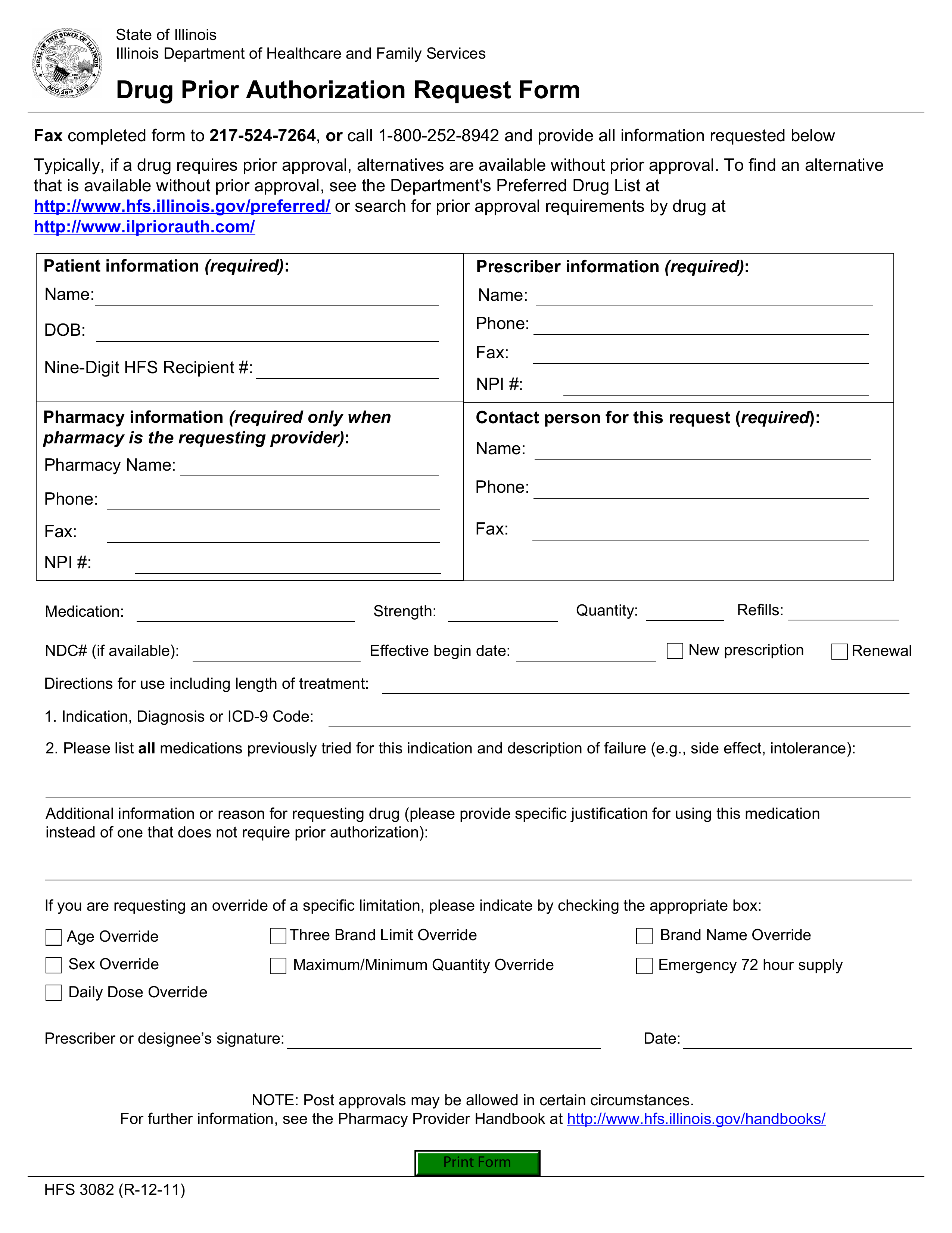
Free Illinois Medicaid Prior (Rx) Authorization Form PDF eForms
Each link will open a new window. You do not need a paper. Determine if a pa is needed with the meridian prior auth check tool. If an authorization is required, submit a request using the secure provider. You must include the most recent relative laboratory results to ensure a complete pa.
Medicare Part B Prior Authorization Form 2024 Ginni Justine
You must include the most recent relative laboratory results to ensure a complete pa. Some covered services or medications may need approval from meridian, and this is called a prior authorization (pa). If an authorization is required, submit a request using the secure provider. Determine if a pa is needed with the meridian prior auth check tool. You do not.
Meridian Health Plan Of Mi Forms
Prior authorization form standard/urgent requests: Some covered services or medications may need approval from meridian, and this is called a prior authorization (pa). Determine if a pa is needed with the meridian prior auth check tool. Each link will open a new window. Use the tool below to see if prior authorization (pa) is needed.
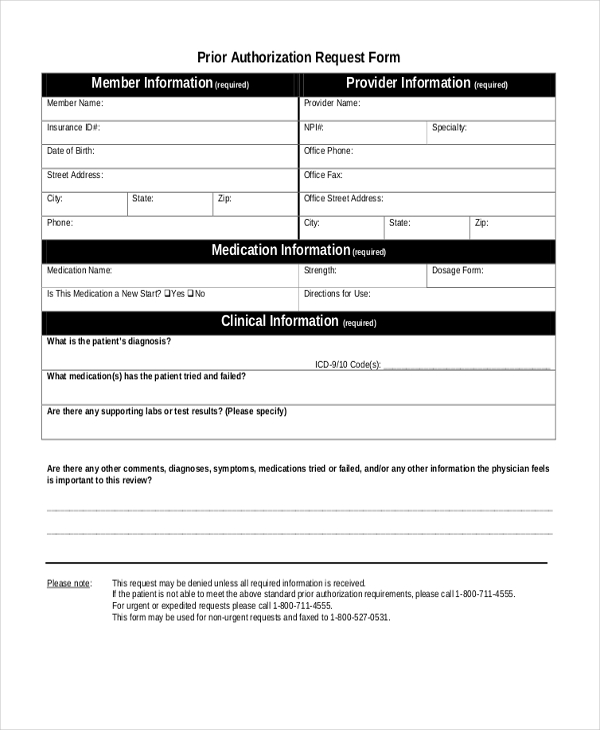
Free Prior (Rx) Authorization Forms PDF eForms
Use the tool below to see if prior authorization (pa) is needed. You do not need a paper. Once you have completed and signed this form,. Prior authorization form standard/urgent requests: Prior authorizations cannot be completed over the phone.
Bcbs Prior Authorization Form Michigan Form Resume Examples kDp3Og030Q
Use this form to ask us to make a coverage determination and/or prior authorization. Each link will open a new window. Determine if a pa is needed with the meridian prior auth check tool. Submit pas electronically through the. How to request a prior authorization.
Fillable Online Bcbs illinois prior authorization form pdf. Bcbs
Some covered services or medications may need approval from meridian, and this is called a prior authorization (pa). Use this form to ask us to make a coverage determination and/or prior authorization. If an authorization is required, submit a request using the secure provider. How to request a prior authorization. Once you have completed and signed this form,.
How Do I Submit A Prior Authorization To Medicare?
How to request a prior authorization. Submit pas electronically through the. Some covered services or medications may need approval from meridian, and this is called a prior authorization (pa). Determine if a pa is needed with the meridian prior auth check tool. Each link will open a new window.
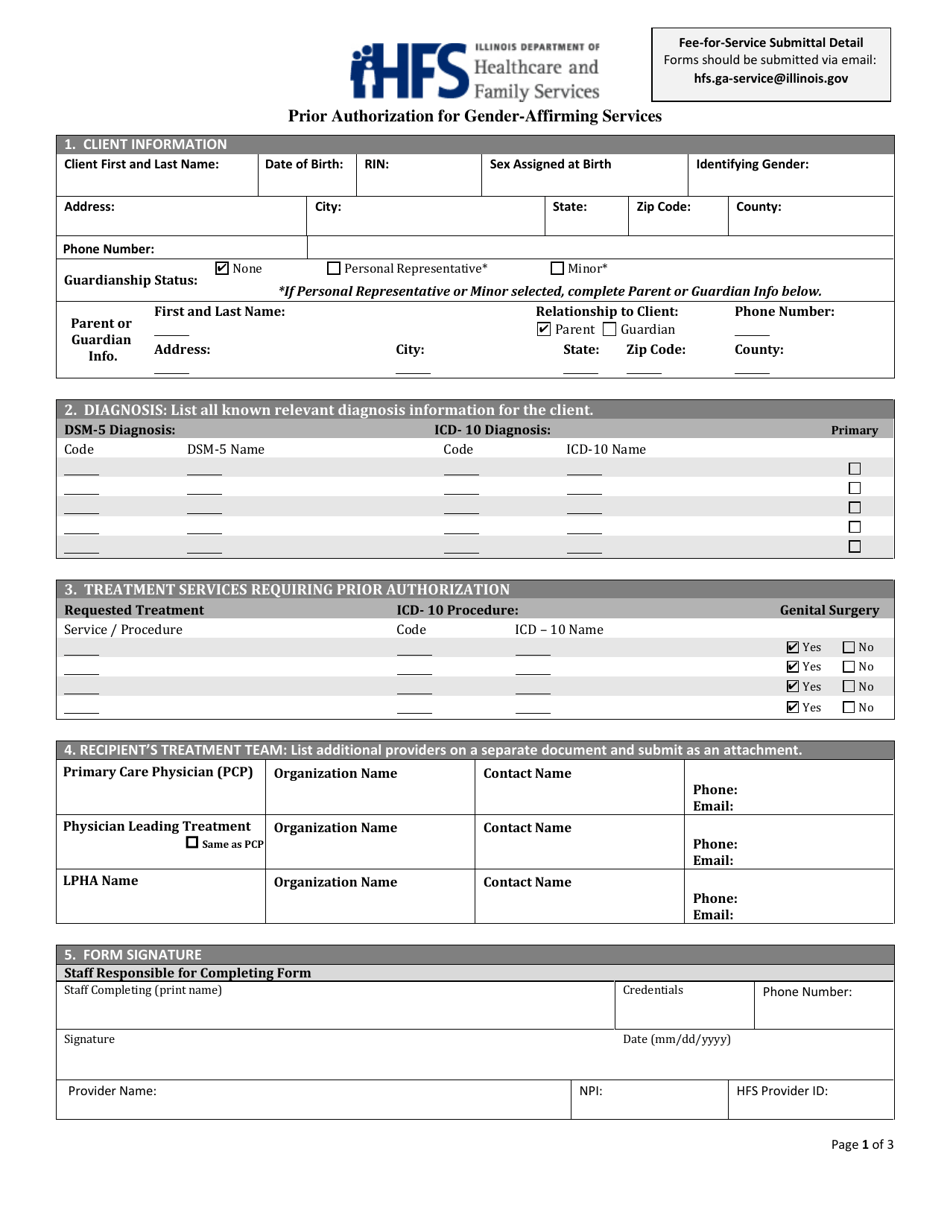
Illinois Prior Authorization for GenderAffirming Services Fill Out
Determine if a pa is needed with the meridian prior auth check tool. Submit pas electronically through the. How to request a prior authorization. Once you have completed and signed this form,. Some covered services or medications may need approval from meridian, and this is called a prior authorization (pa).
Fillable Online Free Meridian Prior (Rx) Authorization Form
Submit pas electronically through the. You do not need a paper. Determine if a pa is needed with the meridian prior auth check tool. Prior authorizations cannot be completed over the phone. You must include the most recent relative laboratory results to ensure a complete pa.
Use The Tool Below To See If Prior Authorization (Pa) Is Needed.
You must include the most recent relative laboratory results to ensure a complete pa. Once you have completed and signed this form,. You do not need a paper. If an authorization is required, submit a request using the secure provider.
Use This Form To Ask Us To Make A Coverage Determination And/Or Prior Authorization.
Submit pas electronically through the. How to request a prior authorization. Prior authorizations cannot be completed over the phone. Each link will open a new window.
Determine If A Pa Is Needed With The Meridian Prior Auth Check Tool.
Prior authorization form standard/urgent requests: Some covered services or medications may need approval from meridian, and this is called a prior authorization (pa).