Meritain Medical Necessity Form
Meritain Medical Necessity Form - Please include any additional comments if needed with. **please select one of the options at the left to proceed with your request. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. To determine whether a benefit is covered or excluded, please review the eligible medical benefits and/or exclusions. Attach all clinical documentation to support medical necessity. Always place the predetermination request form on top of other supporting documentation. The patient’s plan document supersedes this and aetna® clinical. Welcome to the meritain health benefits program. For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while.
Please include any additional comments if needed with. The patient’s plan document supersedes this and aetna® clinical. To determine whether a benefit is covered or excluded, please review the eligible medical benefits and/or exclusions. Welcome to the meritain health benefits program. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. **please select one of the options at the left to proceed with your request. Attach all clinical documentation to support medical necessity. Always place the predetermination request form on top of other supporting documentation. For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item.
For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item. Attach all clinical documentation to support medical necessity. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. The patient’s plan document supersedes this and aetna® clinical. Welcome to the meritain health benefits program. **please select one of the options at the left to proceed with your request. Please include any additional comments if needed with. To determine whether a benefit is covered or excluded, please review the eligible medical benefits and/or exclusions. Always place the predetermination request form on top of other supporting documentation. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you.
About Meritain Health Medical Management YouTube
To determine whether a benefit is covered or excluded, please review the eligible medical benefits and/or exclusions. **please select one of the options at the left to proceed with your request. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. Attach all clinical documentation to support medical necessity. Always place.
Medical Necessity Form Complete with ease airSlate SignNow
To determine whether a benefit is covered or excluded, please review the eligible medical benefits and/or exclusions. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. **please select one of the options at the left to proceed with your request. Always place the predetermination request form on top of other.
Meritain Med Necessity 20192024 Form Fill Out and Sign Printable PDF
Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan.
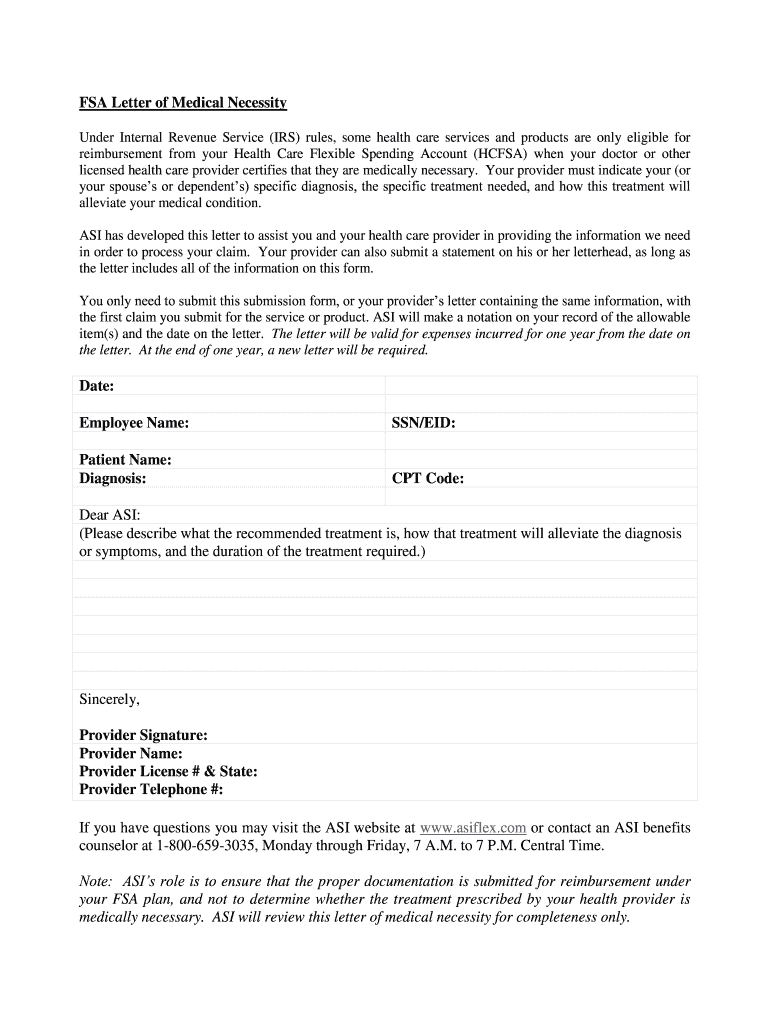
Medical Necessity Letter Template.docx Medical Necessity Letter
Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. **please select one of the options at the left to proceed with your request. Always place the predetermination request form on top of other supporting documentation. Percertification and preauthorization (also known as “prior authorization”) means that approval is required.
Meritain Health All About Medical ID Cards YouTube
The patient’s plan document supersedes this and aetna® clinical. **please select one of the options at the left to proceed with your request. Always place the predetermination request form on top of other supporting documentation. Please include any additional comments if needed with. Welcome to the meritain health benefits program.
Certificate Of Medical Necessity Form Template Get Free Templates
The patient’s plan document supersedes this and aetna® clinical. Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item. Please include any additional comments if needed with. To determine.
Certificate Of Medical Necessity (CMN) For Support Surfaces Fill and
To determine whether a benefit is covered or excluded, please review the eligible medical benefits and/or exclusions. **please select one of the options at the left to proceed with your request. The patient’s plan document supersedes this and aetna® clinical. Welcome to the meritain health benefits program. Please include any additional comments if needed with.
Fillable Online Certificate of Medical Necessity DME 484
Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. Attach all clinical documentation to support medical necessity. Welcome to the meritain health benefits program. Always place the predetermination request form on top of other supporting documentation. The patient’s plan document supersedes this and aetna® clinical.
American Specialty Health Medical Necessity Review Form 20162021
**please select one of the options at the left to proceed with your request. Always place the predetermination request form on top of other supporting documentation. For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item. Please include any additional comments if needed with. The patient’s plan document.
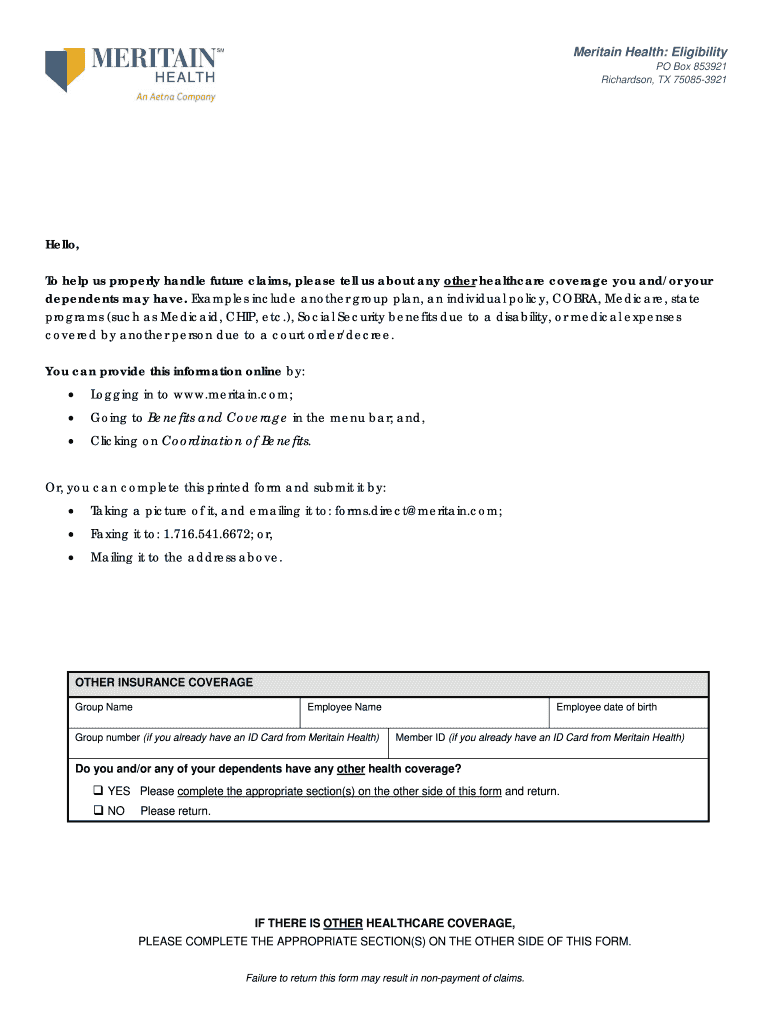
Meritain Health Medical Claim Form
Attach all clinical documentation to support medical necessity. Always place the predetermination request form on top of other supporting documentation. **please select one of the options at the left to proceed with your request. For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item. The patient’s plan document.
Welcome To The Meritain Health Benefits Program.
Please include any additional comments if needed with. The patient’s plan document supersedes this and aetna® clinical. To determine whether a benefit is covered or excluded, please review the eligible medical benefits and/or exclusions. For vitamins and supplements, we must have a letter of medical necessity (lomn) on file, stating the specific need for each item.
Attach All Clinical Documentation To Support Medical Necessity.
Percertification and preauthorization (also known as “prior authorization”) means that approval is required from your health plan before you. Meritain health’s® medical management program is designed to ensure that you and your eligible dependents receive the right health care while. **please select one of the options at the left to proceed with your request. Always place the predetermination request form on top of other supporting documentation.